Director of Public Health annual report 2026
1. Foreword
Healthy weight is essential to the health and happiness of our children and the next generation of adults. Childhood should be a time for exploration, boundless energy and optimism. Yet for too many children their health and future prospects are overshadowed by excess weight. The consequences of excess weight fall on all of us – on individuals, on health services and on the wider economy. And the solution lies with all of us: in the choices we make, the communities we build, and the physical and social environment we create. This is a time for action, collaboration, and hope. Together, we can build brighter futures for our children, one step at a time.
Dr Richard Harling
Director of Public Health for Staffordshire
[IMAGE PLACEHOLDER]
2. Context
2. Context Excess weight is a complex issue. Obesity is classified by the World Health Organization (WHO) as a chronic, relapsing disease arising from complex interactions between genetics, neurobiology, eating behaviours, access to healthy diet, market forces, and the broader environment.
Worldwide, nearly half a billion children – around 1 in 4 - will be overweight or obese by 2030. More than one third of all adults are already living with excess weight.
In the UK, rates of excess weight have been worsening and it is predicted to overtake tobacco as the most significant avoidable cause of illness and death in our population.
Children with excess weight are more likely to experience excess weight as adults. Early onset of obesity increases the risk of serious health conditions such as type 2 diabetes and heart disease during childhood and sets the stage for these chronic diseases to develop or persist into adulthood.
Addressing excess weight in childhood is crucial to the health of the population. It requires a comprehensive approach that considers individual and family choices, social norms, and the wider economic and physical environment.
It is important to strike a careful balance between a focus on individuals and wider society. If we allow excess weight to become normalised we are accepting a profound human and financial cost. At the same time we must avoid stigmatising people living with overweight or obesity: not all of the factors that determine our weight are within our personal control.
The goal should be to create an environment in which healthy choices are the easy choices and a culture of personal responsibility and mutual respect.
- Obesity and overweight
- Prevalence of Obesity | World Obesity Federation
- Recipe for health: a plan to fix our broken food system
- Royal College of Paediatrics and Child Health (2020) State of Child Health. London: RCPCH. Home - RCPCH - State of Child Health
- Children's overweight and obesity - NHS England Digital
Excess weight includes overweight and obesity.
Data on childhood obesity comes from the National Child Measurement Programme, a mandated national programme. Heights and weights of school children are measured in reception and year 6 and used to calculate a Body Mass Index (BMI) centile.
The definitions are:
- Obese: > 95th BMI centile
- Overweight: 85th to 95th BMI centile
- Healthy weight: 2nd to 85th BMI centile
Data on adult obesity comes from Sport England Active Lives Adult Survey data. The definitions are:
- Obese: BMI >30.0
- Overweight: BMI 25.0 to 29.9
- Healthy weight: BMI 18.5 to 24.9
[IMAGE PLACEHOLDER]
3. A growing problem
Excess weight is a growing problem. Over the last thirty years the proportion of children with excess weight in the UK has increased from one quarter to one third, and the proportion of adults from a half to two thirds.
Around 60% of the Staffordshire population now live with excess weight - as shown in Figure 1. On current trends this proportion is expected to grow still further – to around three quarters by 2050. Details of the proportions of children and adults overweight and obese are shown in Figures 1 to 3.
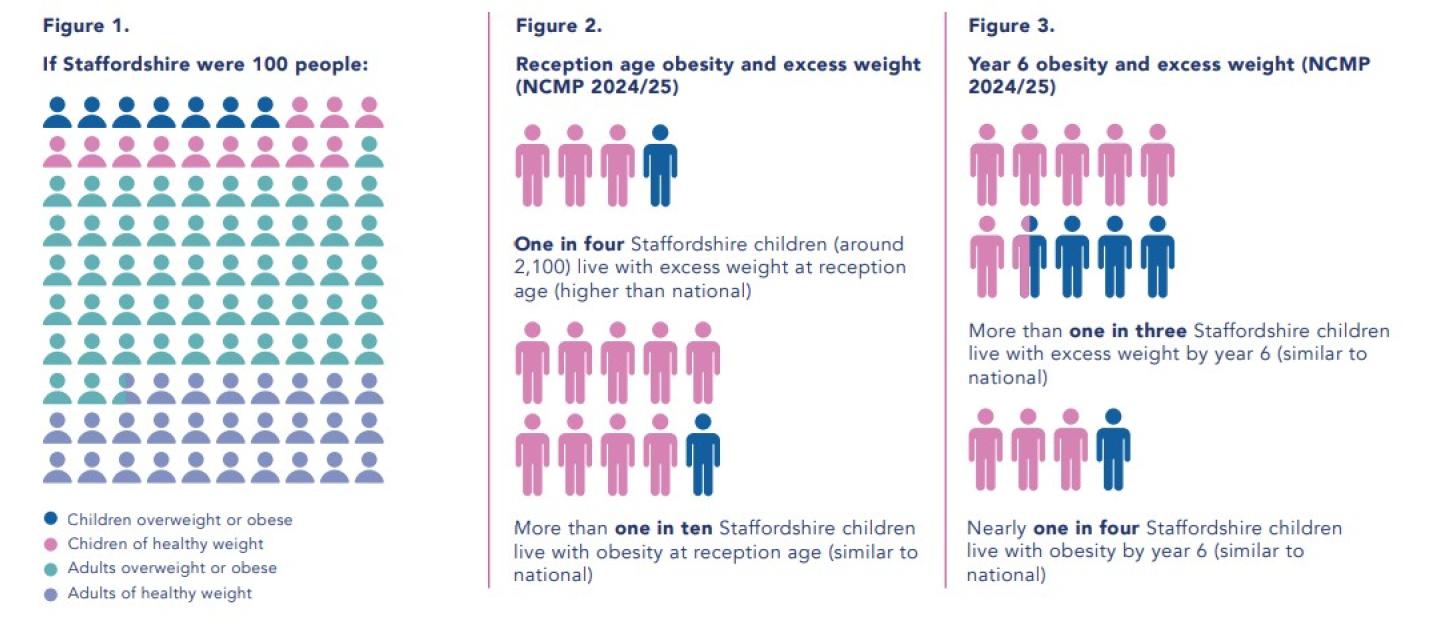
Excess weight is increasing. Over 30 years, excess childhood weight has risen from one quarter to one third, and adult excess weight from one half to two thirds.
Around 60% of Staffordshire now live with excess weight.
On current trends, this could reach three quarters by 2050.
Key points:
• One in four Staffordshire reception children (≈2,100) live with excess weight
• More than one in ten live with obesity at reception age
• More than one in three live with excess weight by Year 6
• Nearly one in four Year 6 children live with obesity
4. With unequal distribution
Excess weight doesn’t affect everyone in our population equally. Some areas of Staffordshire have higher rates of excess weight than others - as shown in figures 4 and 6.
| Area | Obesity | Excess weight |
|---|---|---|
| England | 22.2% | 36.2% |
| Staffordshire | 22.2% | 36.8% |
| Newcastle-under-Lyme | 28.2% | 42.4% |
| South Staffordshire | 22.6% | 37.6% |
| Cannock Chase | 20.6% | 37.4% |
| East Staffordshire | 22.6% | 37.2% |
| Staffordshire Moorlands | 21.3% | 35.4% |
| Stafford | 19.5% | 34.9% |
| Lichfield | 20.2% | 34.8% |
| Tamworth | 21.7% | 33.5% |
There is a relationship between deprivation and excess weight. Analysis of National Child Measurement Programme data shows that all domains of the Index of Multiple Deprivation are strongly associated with excess weight and obesity, especially income, education, and employment7. For example, wards where households have a lower income tend to have higher rates of excess weight, although this does not mean that all wards with lower income have high rates of excess weight or vice versa.
Source: Office for Health Improvement and Disparities. Public health profiles. 2025 https://fingertips.phe.org.uk/ © Crown copyright 2025
Figure 5: Year 6 excess weight by deprivation decile (2022/23, 23/24 and 24/25)
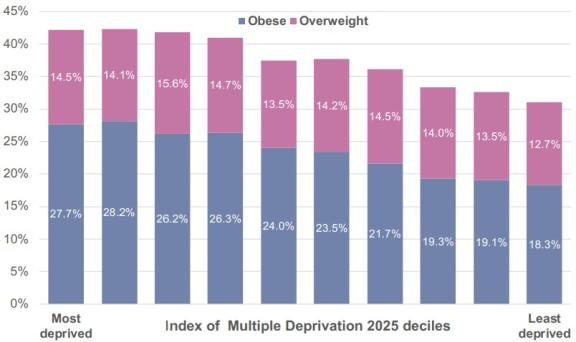
This relationship is shown in Figure 5, with excess weight by individual ward shown in Figure 6. It is because deprivation is a key driver of inequalities in diet, physical activity, access to services, and wider determinants of health, all of which contribute to a higher risk of excess weight
Source: NCMP local dataset 2022/23, 2023/24 and 2024/25, Office for Health Improvement and Disparities. IMD 2025, Ministry of Housing, Communities and Local Government
- Health inequalities for obesity and weight management: a briefing for NICE guideline developers and committee members
- Association of deprivation with overweight and obesity among primary school children in England: an ecological cross-sectional study - The Lancet
5. Why does it matter?
Excess weight is a leading cause of ill health, disability and preventable death.
Excess weight increases the risk of developing a range of serious health conditions including type 2 diabetes, heart disease and stroke, some cancers, and liver disease. The risk increases with the level of excess weight: the heavier people are the greater the risk.
Excess weight also affects quality of life – both for the individual and for wider society. It impairs mobility, mental health and life chances – including people’s ability to work and contribute.
The economic cost is enormous. In the UK, the cost of obesity alone is estimated to be nearly £100 billion each year. Around two thirds of this fall on individuals — through poorer quality of life, the burden of informal care provided by families and friends, and reduced life expectancy. £20 billion is borne by the NHS in treating obesity and related health conditions.
The remaining £15-20 billion is felt across wider society due to reduced academic attainment, benefits, and reduced workforce productivity. Personal Independence Payment claims linked to obesity have increased significantly over the last 5 years8. Lost productivity associated with overweight and obesity combined are estimated to be more than £30 billion in 20309. Relative to healthy weight workers, workers living with overweight take an average of 2.5 additional sickness absence days and workers living with obesity take an average of 5 additional sickness absence days per year
10. The 2024 Director of Public Health Annual Report highlighted the challenge of Staffordshire’s aging population. Between 2021 and 2041 the number of people aged 85 and above will increase by 84% and the number aged 65-84 population by 25%, whilst the number aged 16-64 increases by only 2%. This will lead to a decrease in the ratio of working age to pension age adults from around 2.5 in 2021 to 2.0 in 2041. There will be many more older people requiring care and relatively fewer working age people to pay for it.
On current trends this will be compounded by the growing burden of excess weight. The health conditions caused by excess weight are reducing healthy life expectancy – so the population is not just getting older, it is getting sicker. In addition, the complications of excess weight are reducing the ability of the working age population to remain economically active. Currently, 7% of working age adults are unable to work due to ill health, and as a growing proportion of the population lives with excess weight we can expect this proportion to grow.
Cost of obesity:
- £100 billion/year total to the UK
- £20 billion to the NHS
- £15–20 billion to wider society
- Personal Independence Payment statistics to April 2025 - GOV.UK
- The_economic_and_productivity_costs_of_obesity_and_overweight_in_the_UK_.pdf
- The_economic_and_productivity_costs_of_obesity_and_overweight_in_the_UK_.pdf
6. What are the causes?
Biologically, excess weight accumulates as a result of an imbalance between calories consumed and calories expended. This is a result of people’s choices about what they eat and how much exercise they do.
People’s choices are in turn influenced by the circumstances in which they are born and raised. Dietary habits and exercise levels are determined by wider socio-economic conditions with a whole range of factors influencing the likelihood of excess weight.
We all need to take responsibility, as individuals, parents, families and communities, for the choices that we make. However, fixating solely on individual and parental responsibility ignores the conditions in which people are born, learn and grow.
Many of the factors that determine our weight are outside of our personal control – advertising, availability of healthy food, income, and the design of our towns and cities. Some medical conditions can contribute towards weight gain although this is a relatively minor contribution to excess weight in the population when compared to socioeconomic influences 11. We cannot tackle excess weight solely through exhortations to people to live more healthily; we have to change the environment that sets the context for our choices.
That includes the cultural environment. Excess weight is increasingly becoming normalised. There are parallels with smoking in the 20th century when film stars were used to advertise tobacco products and the environment was adapted to facilitate smoking. We see this mirrored today with celebrities and sports sponsorships used to endorse unhealthy foods, and in the way that we are starting to adapt the environment to respond to people with excess weight. We are starting to lose sight of what a healthy weight is and why is it is important 12.
We must avoid stigmatising people living with overweight or obesity: the psychological and social consequences make the problem worse 13. At the same time we should remember that excess weight is not an aesthetic issue it’s a health issue and should be treated as such – with management of the causes and support for those affected.
Factors Influencing Excess Weight
Excess weight is influenced by a wide range of interconnected factors. These can be grouped into four layers:
1. Genetics (central factor)
At the core are genetic factors, which affect how individuals respond to food, activity levels, and weight‑related behaviours.
2. Individual choices
Surrounding genetics are individual lifestyle choices, such as dietary habits and physical activity behaviours.
3. Social norms
The next layer reflects the influence of social norms, including cultural expectations, behaviours within families and communities, and the social environment people live in.
4. Wider environmental and socioeconomic factors
The outer ring includes broader influences that shape behaviour and opportunity, such as:
- Socioeconomic environment
- Income
- Advertising
- Food availability
- Active travel options
- Green spaces
- Leisure facilities
These wider determinants affect access to healthy foods, opportunities for physical activity, and exposure to unhealthy influences.
- NICE Overweight and Obesity Management Guideline Summary - Guideline Central
- Normalisation of ‘plus-size’ risks hidden danger of obesity | UEA
- Addressing weight stigma - The Lancet Public Health
7. Starting well
Influences on weight start from conception, if not before. Maternal obesity is a key factor influencing childhood health: babies born to mothers with excess weight have an increased risk of excess weight themselves.
The first 1001 days after conception to 2 years build the foundations for lifelong health. Good nutrition during this period promotes the development of a healthy brain and body, including a healthy weight.
Breastfeeding is the best nutrition in early infancy. Staffordshire has low rates of breast-feeding initiation, with 62% of babies receiving their first feed as breast milk compared to 72% nationally. From a low baseline breastfeeding rates fall off quickly with only 43% of babies fed breast milk by 2 months.
Beyond breastfeeding, the introduction of solid foods is a key opportunity to establish healthy food habits. Responsive feeding of infants, based on recognising and responding to their hunger and fullness cues, supports development of a healthy weight. Introducing healthy foods allows infants to learn the tastes and textures associated with healthy eating behaviours.
Parents and carers have a key role in modelling a healthy relationship with food through what and when they choose to eat. Their choices are in turn determined by the environment: social norms, advertising, and the availability and affordability of healthy food14. Many parents are worried about what their children are eating and find it a challenge to feed them healthy food15.
The early years also offer an opportunity to promote exercise. Parents and carers have a key role in developing movement skills, encouraging and facilitating physical activity, and reducing sedentary time16. Again, the wider environment is a key determinant of parental choices: whether they have access to green spaces, leisure facilities, and safe paths and roads for active travel.
Mealtimes Matters CIC…
in 2024/25 trained 28 early years practitioners in 7 primary schools in how to support children and families to develop a healthy relationship with food. More than 90% of children tried new foods, both in school and at home, as well as getting involved in food preparation.
“I think that this programme was brilliant. My child has tried so many new foods and has developed a healthier relationship with food. It definitely helped with mealtimes at home”
(Parent)
8. Learning well
Influences on weight continue through early childhood and into school age. The influence of parents is ongoing, and other influences also come into play – from schools, peers and wider society.
The recent expansion of funded childcare places from 9 months to 4 years of age more children will enter Early Years (EY) settings receiving the majority of their food intake there. Parents also now have the option to provide their child with lunch boxes from home which are often varied in terms of providing children with healthy food and the right portion size for their ages.
School food forms a significant proportion of a children’s food intake. However primary and secondary school children are getting three quarters of their lunchtime calories from ‘ultra-processed foods’ such as frozen pizzas, mass produced sandwiches and fizzy drinks, which are high in calories and low in nutritional value.
Active travel offers an ideal opportunity for children to incorporate exercise into their daily routine. In Staffordshire nearly half of pupils walk, cycle or scoot to school. Barriers include distance, poor infrastructure and perceptions of safety.
Staffordshire Moorlands District Council’s Move More team, surveyed 10 secondary schools to better understand children’s relationship with physical activity.
- 72% of participants said they understand the importance of an active lifestyle with a further 23% saying that they have ‘somewhat’ of an understanding.
- 1 in 3 stated that the main reason for not taking part in activity is ‘lack of time’.
- Half of participants were walking to and from school every day.
- 40% of participants were walking as their main activity at lunchtime, rather than sitting, playing games or playing sport
- 2 out of 3 believe that curriculum PE and school sport helps them to maintain a healthy lifestyle.
The Fun Food Factory ran interactive workshops to year 6 children in Tamworth schools to raise awareness of healthy eating. The feedback was very positive with 90% of children reporting that it made them want to have a go at cooking healthy foods.
“I have learnt that it is not hard to make sure you have a balanced diet, so that you can be healthy”.
“I learnt the food groups I never knew about”.
“We can make food with vegetables, and it tastes good”
“To be healthy and look after your body with what you eat”
“I learnt that every green is nice in some way”
9. Growing well
Advertising has a big influence on children’s food choices. Recent restrictions prevent large retailers from offering multibuy discounts (such as ‘buy one get one free’, 3-for-2 deals or unlimited refills) on foods and drinks high in fat, sugar or salt. Recent restrictions of unhealthy food and drink products on television and online advertising, supported by most parents, could remove up to 7.2 billion calories from children’s diets per year in the UK and reduce the number of children living with obesity by more than 20,000.
Availability and affordability of healthy food are also big factors. Children living in more deprived areas tend to have less access to healthy food. Children living in areas with more ‘fast food’ takeaways are more likely to carry excess weight. Planning regulations offer Local Authorities the power to restrict new openings and control the density of these outlets to improve children’s health.
Focusing on the environment is likely to be a much more sustainable solution than trying to address excess weight through medication. Drugs such as semaglutide may be effective in the short term at helping children with obesity lose weight17. However their longer-term effectiveness is less clear, they do have side effects and they are expensive – and unaffordable for many18. Currently their use is reserved to children aged 12-17 whose obesity is already causing health problems such as breathing difficulties19. Despite what some social media platforms would have us believe20, medication is not a quick fix.
In 2024, South Staffordshire Family Hub provided free fruit to children attending family workshops, encouraging them to explore fruit and vegetables in an interactive and fun way. Locally developed ‘Just add veg’ resources were provided to parents and carers to help with creative food preparation ideas.
“I was amazed when my child, who used to refuse fruit, now can’t get enough of kiwi! It’s a game-changer for us. “
“The ideas we got from the workshops have made mealtimes at home so much fun. We’ve tried dishes from different cultures, and the kids love it!“
“The free fruit initiative is fantastic and was so unexpected. It’s great to see my kids excited about eating healthy.”
- Semaglutide treatment for children with obesity: an observational study - PubMed
- Are weight-loss treatments contributing to health inequalities? - The Health Policy Partnership
- Medicines and surgery | Overweight and obesity management | Guidance | NICE
- Worrying rise of Ozempic & Wegovy ‘transformation’ videos on TikTok
10. Better Health Staffordshire
Partners in Staffordshire have committed to tackle excess weight through a collective approach called ‘Better Health Staffordshire’. Local government, the NHS, the voluntary sector and communities are working together and some fantastic work is ongoing.
Partners across Staffordshire work together to tackle excess weight through Better Health Staffordshire.
Mission:
- Tackle the causes of excess weight, physical inactivity and poor diet
- Enable and empower individuals, families and communities to move more, eat a healthy balanced diet and maintain a healthy weight
Goals:
- Reduce excess weight in children and adults
- More children and adults eating healthy, balanced diets
- More physical activity in children and adults
- Less physical inactivity in children and adults
A whole system approach: creating the conditions for change. ‘Everyone has a role to play’
- Develop a shared understanding of data, insight and evidence
- Develop effective ways of working with partners and communities
- Create healthy settings and environments
- Develop effective information, advice and guidance
- Evaluate impact and embed learning
How stakeholders can engage
- Commit to the mission
- Connect with colleagues, partners and communities
- Champion the approach
- Collaborate on creating the conditions for change
Factors that impact our weight, how active we are and what we eat
- Deprivation
- Income
- Financial security
- Childhood experiences
- Food prices
- Food advertising and promotion
- Genetics and biology
- Stigma
- Mental health
- Sleep
- Access to support and treatment
- Access to opportunities to be physically active
Benefits of the BHS programme
- Improves physical and mental health
- Reduces absence from work
- Physical activity can help prevent anti-social behaviour
- Reduced school absence and better concentration
- Reduction in future health & adult social care costs
11. What we do
| Workstream | How this will help | Examples of what BHS is doing |
|---|---|---|
| Healthy settings and environments | Support positive food experiences and ensure everyone has access to good food Provide spaces for people to be more active as part of everyday life |
|
| Information, advice & guidance (IAG) | Provide access to information and advice that support healthy choices Raise awareness of self-help tools and weight management services |
|
| Partnerships and communities | Partnerships provide coordinated action through a shared understanding of the issue. They ensure communities are involved in shaping local actions |
|
| Data, insight and evidence | A shared understanding of data, insight and evidence enables partners to act collectively and make sure we’re listening to what local people need and want |
|
| Measuring impact and embedding learning | Ensure that we learn, adapt and improve over time |
|
Contact us
Share your achievements, tell us about your ideas or ask us a question at: betterhealthstaffordshire@staffordshire.gov.uk
12. Recommendations for further action
| Stakeholder | Recommendation |
| Individuals and families |
|
| Schools, communities and early years settings. |
|
| Local statutory organisations |
|
| National government |
|
